This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome
65 year old male came to causality with chief complaints
Pain in the lower abdomen for 5 days
Shortness of breath for 5 days
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 25 years back then he had a cough that was blood-stained when he was diagnosed with Tuberculosis ( by what test??) and was on ATT for 6 months after he was said that he is free from the disease.
Then
2 years back then he started having shortness of breath Grade 2 ( sob on some physical activity) which is insidious in onset and relieved temporarily on medication ( drug - unknown; dose unknown; indication - unknown ) from then he had intermittent shortness of breath which relieved on the medication temporarily.
6 months back he again developed shortness of breath of grade 2 ( walking after 300 m ) which is insidious in onset where he was taken to a higher center where he was prescribed a medication that he didn’t use properly and used only on the aggravation of shortness of breath.
After that 5 months back he suffered from an accident where his left tibia and left rib ( which rib???) got fractured where he was managed with POP casting for 45 days and on calcium tablets ( dose -500mg).
He also developed shortness of breath 5 days which was insidious in onset grade 3 ( sob on normal physical activity) which was relieved on medication ( drug unknown; dose - unknown)
There is a history of cough which is productive ( which has mucous as content scanty in quantity; white in colour; and no foreign bodies)
fatigue; sweating ;
No history of palpitations
No H/O fever, or joint pains.
PAST HISTORY
History of pulmonary TB 25 yrs back
No history of DM
No history of Hypertension, asthma, epilepsy, TB
No history of prolonged hospital stay
No history of previous surgeries
PERSONAL HISTORY
Appetite - Reduced since 1 year
Diet - Mixed
Bowel and Bladder - Regular
Sleep - inadequate
Addictions - stopped 20 years back, before alcohol and smoking
Patient is conscious , coherent and co operative and well oriented to time , place and person
No, Icterus, cyanosis, clubbing
generalized lymphadenopathy and no pedal edema
INVESTIGATIONS:
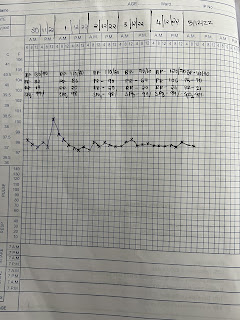
Fever chart
2D echo
Chest X ray
ECG

PROVISIONAL DIAGNOSIS
Pain abdomen under evaluation
Heart failure with mid range reduced ejection fraction (52%)
with Anemia under evaluation with Chronic kidney disease
with a history of Pulmonary TB- 25 years back
TREATMENT
1.INJ HEPARIN 500 IU /IV/QID
2.TAB CLOPIDOGREL - A (150/75) /PO/OD
3.TAB ATORVASTATIN 20mg/PO/HS
4.INJ METROGYL 100ml(500mg)/IV/TID
5.TAB MET - XL 25mg /PO/OD
6.TAB SPOROLAC -DS PO/TID
7.ORS Sachets







Comments
Post a Comment