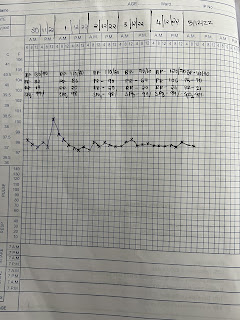
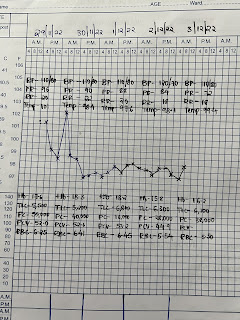
A 58 year old male with headache
58 year old male came with Chief complaints: C/O HEADACHE FRONTAL REGION H/O LOSS OF SPEECH AND LOSS OF CONSCIOUSNESS FOR 1 HOUR IN THE AFTERNOON AT 11:00AM C/O COUGHING OUT BLACK COLOURED SPUTUM SINCE EVENING (9:30PM) > E episodes C/O SWAYING TO RIGHT SIDE SINCE AFTERNOON C/O HICCUPS SINCE NIGHT (9:30PM) C/O DIFFICULTY IN SWALLOWING AND HOARSENESS OF VOICE SINCE AFTERNOON HISTORY OF PRESENTING ILLNESS: PT WAS APPARENTLY ASYMPTOMATIC TILL TODAY AFTERNOON THEN HE DEVELOPED HEADACHE WHICH WAS FOLIO ONLATEY LOSS OF SPEECH AND FOLLOWED BY LOSS LA CONSCIOUSNESS FOR ONE HOUR. FROM EVENING PATIENT STARTED COUGHING BLACK COLOURED SPUTUM (47 EPISODES). PAST HISTORY: K/C/O HTN SINCE 2-3 YEARS ON REGULAR MEDICATION ( T. TELMISARTAN 40MG + T.CLINIDIPINE 10MG) K/CIO DM-II SINCE 2-3 YEARS ON IRREGULAR MEDICATION ADDICTIONS- ALCHOHOL SINCE 30 YEARS SMOKING SINCE 30 YEARS O/E- PT IS CIC/C VITALS-BP-210/140 MMHG PR-116BPM RR-22CPM TEMP-101.1F SP02-94%AT RA GRBS-197MG/DL PALLOR-RESENT ICT...