80 year old male
80yr old male patient with SHORTNESS OF BREATH
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 80 year old male patient was brought to casualty(i.e4/10/2022)
CC:
Shortness of breath since 4days
Fever since 4days
Cough since 3days
Loose stools 2days
History of present illness:
Patient was apparently symptomatic 1 month back then he developed anuria for which he was admitted in a hospital for a day foleys was placed and medication was given for 10 days ,then patient developed shortness of breath four days back which was insidious in onset gradually progressed from grade 2 to grade 4 (mmrc),no postural variation ,no history of suggestive of paroxysmal nocturnal dyspnoea, chest pain ,associated with cold and cough ,cough was productive, sputum mucoid,whitish,copious and not blood tinged and has a history of fever which was intermittent ,on and off ,no diurnal variation and associated with loose stools and burning micturition ,loose stools since two days 3 to 4 episodes per day ,non-bulky not associated with pain abdomen ,non-bloodstained .
Past history:
No similar complaints in the past
Not a know case of DM,ASTHMA,HTN,EPILEPSY,TB
Personal history:
Diet:mixed
Appetite:normal
Bowel and bladder movements:irregular (loose stools), decreased urine output since 1month
Addictions: alcohol consumption from past 30years (daily quarter) stopped 1 month back , last intake was 5 days back
Smoking (Chutta) daily 4-5 , stopped 5 years back
No know allergies
Family history:
No relevant family history
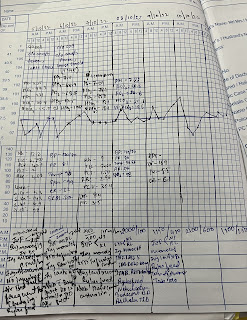
Fever chart:
General Examination:
Patient was not C/C/C not oriented to time,place and person
Pallor -absent
Icterus-absent
Cyanosis-absent
Clubbing-absent
Lymphadenopathy-absent
Edema-absent
VITALS:
BP - 120/70 MM HG
PR-88 BPM
RR-27CPM
SPO2 - 97%
GRBS: 115mg/dl
TEMP - 98.2F
Systemic examination:
RS:
Inspection :
R. L
Supraclavicular area :hollow. Normal
Infraclavicular area. :Crowding Normal
Position of trachea :prominent SCM on rigth side
Position of Apex beat :5 th ics
Chest : asymmetry
Increased AP diameter on left side
Palpation:
Confirmed inspiratory finding
CVS:
Apex beat at 5th ics at midclavicular line
S1,S2 heard
Per abdomen:
Scaphoid
Scar + rt side( h/o? hernia sx)
INVESTIGATIONS:
On 14/10/22
On 15/10/22
On 16/10/22
On 17/10/22
PROVISIONAL DIAGNOSIS:
Altered Sensorium ( hypoactive) secondary to ? Uremic Encephalopathy
T - || respiratory failure?
Uremic Encephalopathy
Oliguric AKI (resolving)
with Right Upper Lobe Fibrosis ( fungal ball) ? Mass @Rt lung with ?
Left lower lobe ASPIRATION PNEUMONIA
With ? MAT ? AF sinus arrhythmia
Post dialysis done (1st - 6/10/22
2nd - 11/10/22 , 3rd - 13/10/22 , 4th - 15/10/22)
TREATMENT:
12/10/22
O: Patient on Mechanical Ventilator
Mode: CPAP VC
FiO2 : 30
PEEP: 7
Temp-99.5°F
BP- 90/50 MMHG
PR-67 BPM
RR-22 CPM
CVS-S1S2+
RS: BAE+
Crepts + Left infra axillary added sounds @ left infclavicular, right mammary
P?/A : soft, non- tender
SPO2 - 98%
GRBS: 138mg/dl
GCS: E1VTM1
A:
Altered Sensorium ( hypoactive) secondary to T-II respiratory failure?
Uremic Encephalopathy
Oliguric AKI (resolving)
with Right Upper Lobe Fibrosis ( fungal ball) ? Mass @Rt lung with ?
Left lower lobe ASPIRATION PNEUMONIA
With ? NAF With ? AF With ? BEDSORE - 2
Yesterday dialysis done (2nd session)
P:
1. IVF NS and RL @ 50mL /hr
2. INJ.MEROPENEM 1g/ IV/BD
3. INJ. LASIX 80mg /IV /BD
4. INJ NOR ADRENALINE (2amp + 46ml ns @ 5ml/hr acc to Bp
5. INJ ATRACURIUM @ 2ml/hr
6. INJ MIDAZOLUM @ 2ml/hr
7.Ryles feed - milk (100 mL+ protein powder) 4th hourly
water - 100mL 6th hourly
8.TAB. AZITHROMYCIN 500mg /RT/OD
9. TAB. DOLO 650mg/RT/SOS if temp. more than 101F
10.Air bed
11.Nebulisation
- Budecort /BD/12th hourly
- Asthalin / TID/ 8th hourly
12.Frequent position change
13.Daily Bed sore dressing
14.Monitor vitals BP, Temp, PR, RR, SpO2 hourly
15.GRBS charting 2nd hourly
16. Strict I/O charting
17.Inform SOS
13/10/22
O: Patient on Mechanical Ventilator
Mode: CPAP VC
GCS: E2VTM1
Temp-98.7
BP- 100/50MMHG
PR-94 BPM
RR-41 CPM
CVS-S1S2+
RS: BAE+
Crepts + Left infra axillary added sounds @ left infclavicular, right mammary
P/A : soft, non- tender
SPO2 - 99%
GRBS: 134mg/dl
A:
Altered Sensorium ( hypoactive) secondary to T-II respiratory failure?
Uremic Encephalopathy
Non Oliguric AKI (resolving)
with Right Upper Lobe Fibrosis ( fungal ball) ? Mass @Rt lung with ?
Left lower lobe ASPIRATION PNEUMONIA
With ? NAF With ? AF With ? BEDSORE - 2
Post dialysis done (1st - 6/10/22
2nd - 11/10/22)
Bed sore dressing done yesterday
P:
1. IVF NS and RL @ 50mL /hr
2. INJ.MEROPENEM 1g/ IV/BD
3. INJ. LASIX 80mg /IV /BD
4. INJ NOR ADRENALINE (2amp + 46ml ns @ 5ml/hr acc to Bp
5.Ryles feed - milk (100 mL+ protein powder) 4th hourly
water - 100mL 6th hourly
6.TAB. AZITHROMYCIN 500mg /RT/OD
7. TAB. DOLO 650mg/RT/SOS if temp. more than 101F
8.Air bed
9.Nebulisation
- Budecort /BD/12th hourly
- Asthalin / TID/ 8th hourly
10.Frequent position change
11.Daily Bed sore dressing
12.Monitor vitals BP, Temp, PR, RR, SpO2 hourly
13.Strict I/O charting
14.Inform SOS
14/10/22
O: Patient on Mechanical Ventilator
Mode: CPAP VC
GCS: E3VTM4
Temp-99F
BP- 140/80MMHG
PR-93 BPM
RR-34 CPM
CVS-S1S2+
RS: BAE+
Crepts + Left infra axillary added sounds @ left infclavicular, right mammary
P/A : soft, non- tender , no organomegaly
SPO2 - 96%
GRBS: 99mg/dl
A:
Altered Sensorium ( hypoactive) secondary to T-II respiratory failure?
Uremic Encephalopathy
Oliguric AKI
with Right Upper Lobe Fibrosis ( fungal ball) ? Mass @Rt lung with ?
Left lower lobe ASPIRATION PNEUMONIA
With ? MAT ? AF sinus arrhythmia
Post dialysis done (1st - 6/10/22
2nd - 11/10/22 , 3rd - 13/10/22)
P:
1. IVF NS and RL @ 50mL /hr
2. INJ.MEROPENEM 1g/ IV/BD in 50ml ns
3. INJ. LASIX 80mg /IV /BD
4.Ryles feed - milk (100 mL+ protein powder) 4th hourly
water - 100mL 6th hourly
5.TAB. AZITHROMYCIN 500mg /RT/OD
6. TAB. DOLO 650mg/RT/SOS
7.Air bed
8.Nebulisation
- Budecort /BD/12th hourly
- Asthalin / TID/ 8th hourly
9.Frequent position change
10.Daily Bed sore dressing
11.Monitor vitals BP, Temp, PR, RR, SpO2 hourly
12.Strict I/O charting
13.Inform SOS
15/10/22
O: Patient on Mechanical Ventilator
Mode: CPAP VC
GCS: E2VTM1
Temp-98.7F
BP- 140/80MMHG
PR-102 BPM
RR-46CPM
CVS-S1S2+
RS: BAE+
Crepts + Left infra axillary added sounds @ left infclavicular, right mammary
P/A : soft, non- tender , no organomegaly
SPO2 - 94%
GRBS: 92mg/dl
A:
Altered Sensorium ( hypoactive) secondary to ? Uremic Encephalopathy
T - || respiratory failure?
Uremic Encephalopathy
Oliguric AKI (resolving)
with Right Upper Lobe Fibrosis ( fungal ball) ? Mass @Rt lung with ?
Left lower lobe ASPIRATION PNEUMONIA
With ? MAT ? AF sinus arrhythmia
Post dialysis done (1st - 6/10/22
2nd - 11/10/22 , 3rd - 13/10/22)
P:
1. IVF NS and RL @ 50mL /hr
2. INJ.MEROPENEM 1g/ IV/BD in 50ml ns
3. INJ. LASIX 80mg /IV /BD
4.Ryles feed - milk (100 mL+ protein powder) 4th hourly
water - 100mL 6th hourly
5.TAB. AZITHROMYCIN 500mg /RT/OD
6. TAB. DOLO 650mg/RT/SOS
7.TAB AZITHROMYCIN 500mg/RT/OD
8.TAB METXL 12.5mg/RT/OD
9.Air bed
10.Nebulisation
- Budecort /BD/12th hourly
- Asthalin / TID/ 8th hourly
11.Frequent position change
12.Daily Bed sore dressing
13.Monitor vitals BP, Temp, PR, RR, SpO2 hourly
14.Strict I/O charting
15.Inform SOS
16/10/22
O: Patient on Mechanical Ventilator
Mode: ACMV - VC
GCS: E3VTM5
Temp-98.2F
BP- 120/70MMHG
PR-88 BPM
RR-27CPM
CVS-S1S2+
RS: BAE+
Left basal crepts
P/A : soft, non- tender , no organomegaly
SPO2 - 97%
GRBS: 115mg/dl
A:
Altered Sensorium ( hypoactive) secondary to ? Uremic Encephalopathy
T - || respiratory failure?
Uremic Encephalopathy
Oliguric AKI (resolving)
with Right Upper Lobe Fibrosis ( fungal ball) ? Mass @Rt lung with ?
Left lower lobe ASPIRATION PNEUMONIA
With ? MAT ? AF sinus arrhythmia
Post dialysis done (1st - 6/10/22
2nd - 11/10/22 , 3rd - 13/10/22 , 4th - 15/10/22)
P:
1. IVF NS and RL @ 50mL /hr
2. INJ.MEROPENEM 1g/ IV/BD in 50ml ns
3. INJ. LASIX 80mg /IV /BD
4.Ryles feed - milk (100 mL+ protein powder) 4th hourly
water - 100mL 6th hourly
5. INJ ATRACURIUM (2amp+45ml NS) @ 5-10ml/hr
6. TAB. DOLO 650mg/RT/SOS
7.TAB AZITHROMYCIN 500mg/RT/OD
8.TAB METXL 12.5mg/RT/OD
9.TAB AKT3(2tab) + pyrazinamide 750mg ( 1tab)
10.Air bed
11.Nebulisation
- Budecort /BD/12th hourly
- Asthalin / TID/ 8th hourly
12.Frequent position change
13.Daily Bed sore dressing
14.Monitor vitals BP, Temp, PR, RR, SpO2 hourly
15.Strict I/O charting
16.Inform SOS















Comments
Post a Comment